Background

The Mobility Saves Project was initially created to showcase a major study commissioned by the Amputee Coalition and conducted by Dr. Allen Dobson, health economist and former director of the Office of Research at CMS (then the Health Care Financing Administration), which shows that the Medicare program pays more over the long-term in most cases when Medicare patients are not provided with replacement lower limbs, spinal orthotics, and hip/knee/ankle orthotics.
Lower extremity and spinal orthotic and prosthetic devices and related clinical services are designed to provide stability and mobility to patients with lower limb loss or impairment and spinal injury. Supplying bracing or support (an orthosis) where needed or a new artificial limb (prosthesis) when necessary saves our healthcare system significant future costs. Medicare’s own data shows this to be the case. Timely treatment that preserves or helps regain mobility not only makes sense; it also saves dollars.
The Mobility Saves project now serves to promote research that further proves that Mobility Saves.
The Dobson DaVanzo Study (2007-2010)
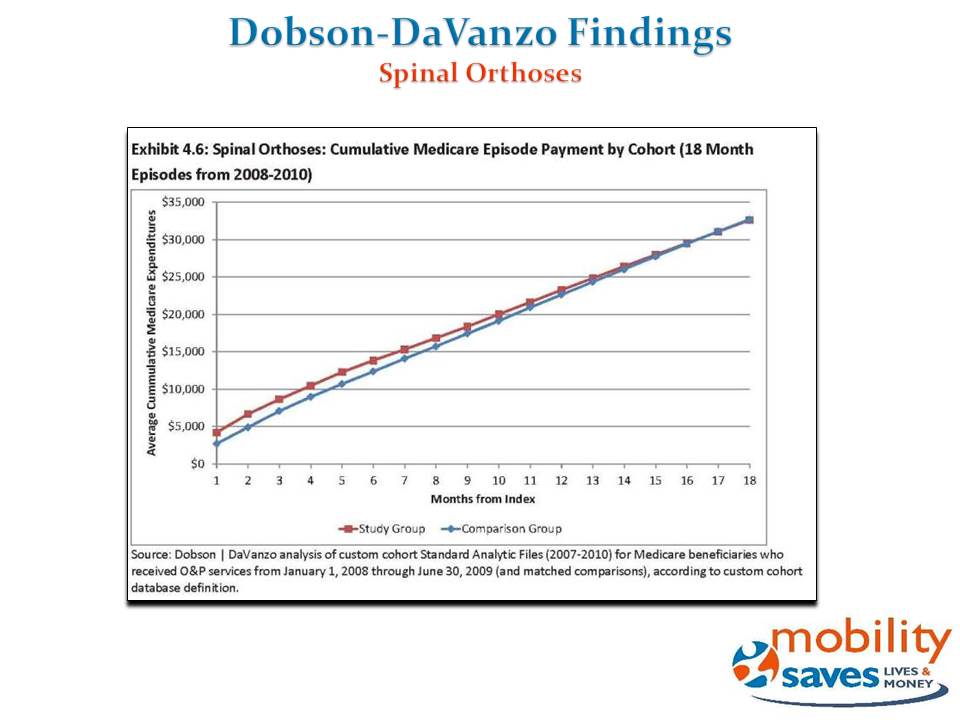
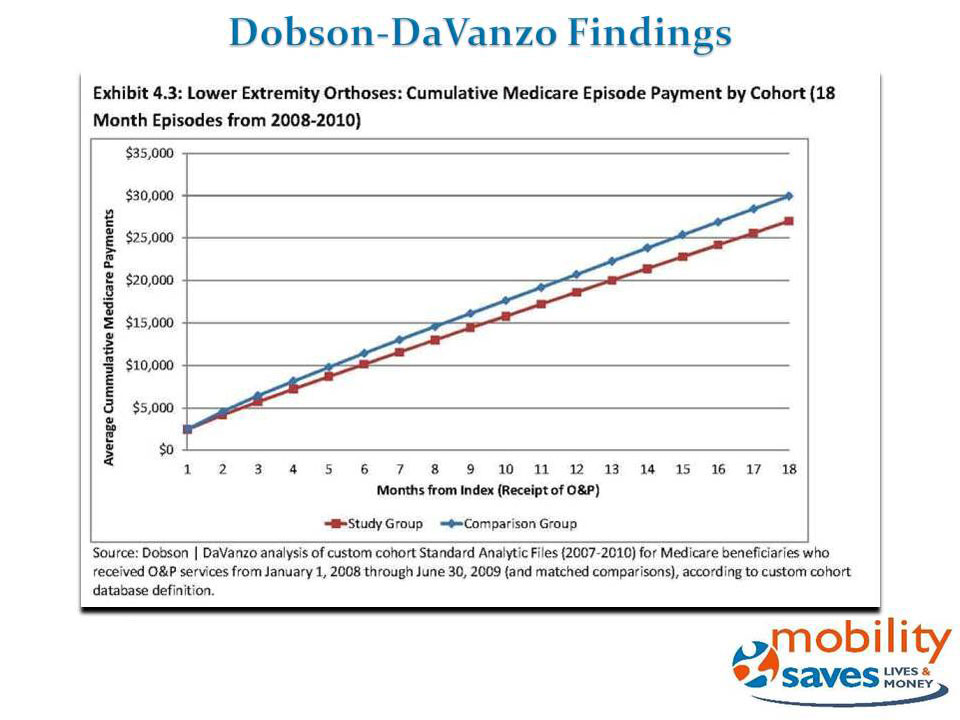
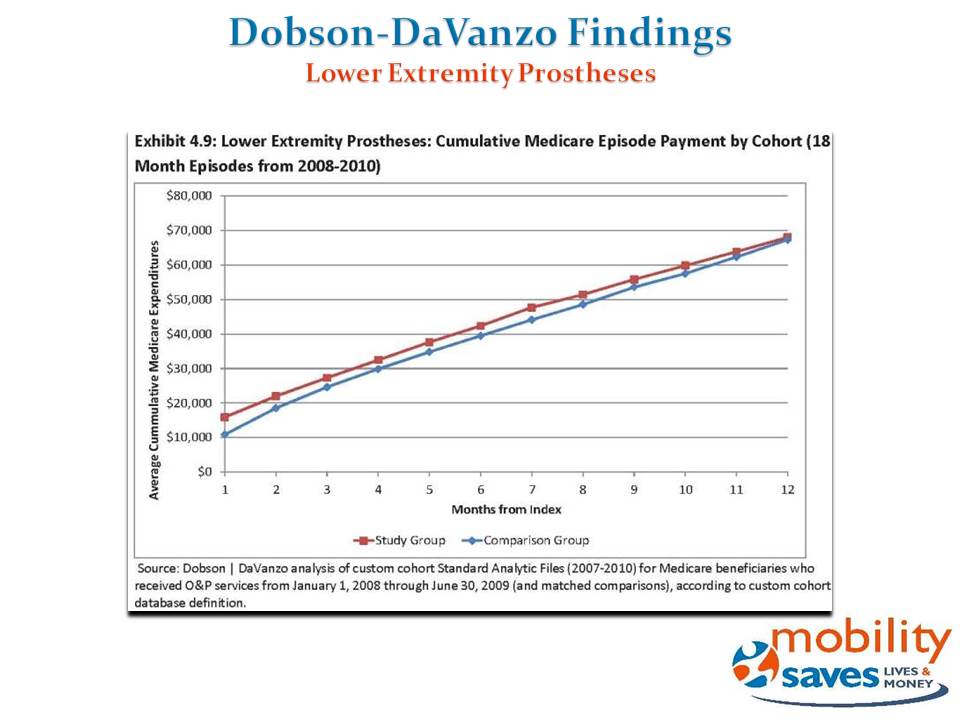
The study’s authors used the Medicare Claims database to review all Medicare claims data for patients with conditions that justified the provision of lower limb orthoses, spinal orthoses, and lower limb prostheses. The unprecedented study looked at nearly 42,000 paired sets of Medicare beneficiaries with claims from 2007-2010. The paired patients either received orthotic and prosthetic care or they did not get such care.
Results
The study’s key finding was that Medicare costs are lower or similar for patients who received orthotic or prosthetic services, compared to patients who need, but do not receive, these services. According to the study, Medicare could save 10 percent ($2,920 on average) for those receiving lower extremity orthoses, and there also are modest savings for patients receiving spinal orthoses and lower extremity prostheses.
New Studies
The RAND Report
Due to recent advances in technologies, prosthetic knees and feet allow for more dynamic movements and improve user quality of life, but payers have recently started questioning their value for money. To answer this question, RAND Corporation simulated the differential clinical outcomes and cost of microprocessor-controlled knees (MPK) compared to non-microprocessor controlled knees (NMPK). They conducted a literature review of the clinical and economic impacts of prosthetic knees, convened technical expert panel meetings, compiled the input parameters required, and constructed and implemented a simulation model over a 10-year time period for unilateral transfemoral Medicare amputees with a Medicare Functional Classification Level of 3 and 4.
Results
RAND found that compared to Non MPK, MPK is associated with sizeable improvement in physical function and reductions in incidences of falls and osteoarthritis. The effect on low-back pain, depression, obesity, diabetes, and cardiovascular disease could not be quantified due to the lack of data. The simulation results show that over a 10-year time-period, compared to NMPK, MPK is associated with an incremental cost of $10,604 per person and an increase of 0.91 quality adjusted life year per person, resulting in an incremental cost of $11,606 per quality adjusted life year gained. The results suggest that the incremental cost of MPK is in line with commonly accepted criteria for good value for money and with the incremental cost of other medical devices that are currently covered by U.S. payers.
Dobson DaVanzo (2011-2014)
Referencing the previously noted Dobson and DaVanzo study, this study reports on a parallel analysis based on claims from 2011-2014 and includes Medicare Part D drug claims in addition to Parts A and B. Its purpose is to validate earlier conclusions on the extent to which Medicare patients who received select orthotic and prosthetic services had less total health care utilization, lower Medicare payments, and/or fewer negative outcomes compared to matched patients not receiving these services.
Results
These outcomes generally echoed those found in the prior study, with some fluctuation in the dollar spread between the study and comparison groups in specific subcategories of expenditures. Across all analyses, the results suggest that orthotic and prosthetic services provide value to the Medicare program and to the patient. Patients who received lower extremity orthotics had total 18-month episode costs that were $1,939 lower than comparable patients who did not receive orthotic treatment ($22,734 vs $24,673). Patients who received spinal orthotic treatment had total 18-month episode costs that were $2,094 lower than comparable patients who did not receive orthotic treatment ($23,560 vs $25,655). Study group beneficiaries receiving both types of orthotics had significantly lower Part D spending than those not receiving treatment. Patients who received lower extremity prostheses had comparable Medicare episode payments to matched beneficiaries not receiving prostheses ($68,877 for study group, $68,893 for comparison group) despite the relatively high cost of the prosthesis, and better outcomes on select metrics. Prosthetic study group patients had significantly lower spending for most facility-based care, o setting the cost of the prosthetic over a 15-month period.Video News Release